SCAR WARS: AN ARTICLE ON LIVER CIRRHOSIS
By Deniz Kaya
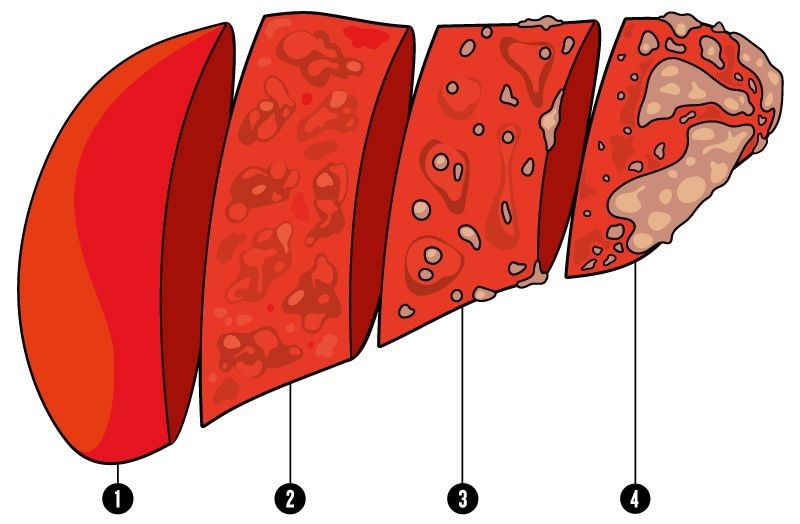
Stages of fibrosis, leading to cirrhosis
Scarring of the liver is due to long term damage to the organ, which leads to a condition known as fibrosis. This fibrosis occurs when the liver attempts to repair and replace damaged cells, resulting in the build up of large quantities of scar tissue over time, if the main cause is not dealt with effectively. Though the build up of this scar tissue causing fibrosis is not bad by itself, as the severity of scarring increases, we can begin to see the result of cirrhosis, in which the liver cells gradually give way to tougher and less functional scar tissue, the organ eventually losing its function all together.
This condition can result in permanent damage to the liver, including a greatly increased risk of liver cancer, and a variety of other different problems, symptomatic of an improperly functioning or failing liver. According to the NHS, this involves, “Yellowing of the skin and whites of the eyes (jaundice), vomiting blood, itchy skin, dark, tarry looking faeces, a tendency to bleed or bruise more easily, swollen legs (oedema) or tummy (ascites) from a build up of fluid,” and more.
It is a disease that claims an estimated million, world-wide, annually.
However, new research into combative drugs are underway, which utilise the natural mechanisms of the liver, which already provides a means of degrading scar tissue and regenerating healthy tissue over time.
It is this mechanism, that has spurred new research into new drugs that are able to halt the progression of the liver scarring or to speed up the healing of the liver once the external causes of the condition have been removed.
Of course, the removal of these external causes or risk factors is the most effective way of making sure the disease has no effect, by making sure that it is never able to occur in the first place, but finding new ways of treating the disease once it has been discovered is of priority for researchers.
The current research involves finding out more about the biology of the scar causing cells and how they work, in order to create a way of reducing the amount of scarring tissue present within the liver. These cells, known as myofibroblasts, work by secreting collagen at injury sites of the liver and then forming a mesh using the cross link of these collagen fibres. This network of collagen fibres will then stiffen and block up the site of the injury.
It is the relatively new understanding of how these myofibroblasts act that has allowed therapeutic intervention to occur, in order to prevent the formation of later onset diseases, such as cirrhosis, and the inevitable consequence of an improperly functioning or failing liver.
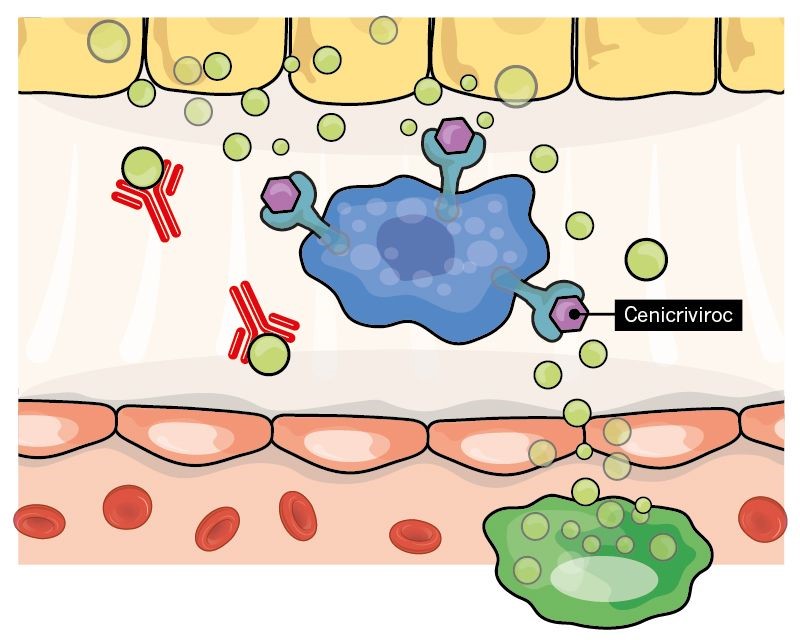
One such solution involves making sure that the myofibroblasts are not able to be activated, which is what prompts their action within the formation of the scar tissue in the first place. This is done through having a focus on the messenger chemicals, cytokines, which are released by damaged liver cells at the site of injury and immune cells which also signal the activation of myofibroblasts by blocking receptors for profibrosis messengers.
Effect of Cenicriviroc on cell signalling
An example of this includes a new drug known as Cenicriviroc, which is surprisingly more well known as an experimental treatment for HIV.
However, the Department of Health and Human Services for the US, show the additional treatment of Nonalcoholic steatohepatitis or NASH, for short, which is a disease caused due to a build up of fat within the liver, which is also one of the main causes of scarring.
Another popular alternative involves the inactivation of the myofibroblasts, by making sure that cytokines are unable to bind to the chemical receptors on their surface, called integrins, which allow further interaction with other myofibroblasts and the extracellular matrix of the cell, of which the collagen fibre mesh acts upon.
These types of drugs are more close to being safe for release for the general market, and are nearing the beginning of human testing within clinical trials.
The next treatment, involves not affecting the cytokines which prompt myofibroblast activation or the intergrins on their surface, but going into the cell to prevent their ability to form the collagen fibres, which lead to tissue scarring in the first place.
These types of drugs work by inserting small sections, so genes, of RNA, into myofibroblasts, preventing the machinery that leads to collagen fibre formation from working.
Finally, there is a type of drug which has no effect on myofibroblasts but instead acts on the cross linking mechanism of the collagen fibres, preventing the formation of a mesh. It does this by blocking the enzymes that cause this cross linking to happen, leading to an easier process of degradation by the body.
Though all of the above therapies are currently in development and will require long periods of clinical trials, it is likely that this period of testing will be lengthened, due to the slow and progressive nature of fibrosis of the liver. This means that new methods will need to be developed, in order to increase the efficiency of current clinical trials, to ensure that vital treatments to serious diseases are delivered to the general market more quickly and effectively.
This comes down to the final new development of biomarkers, which may be able to speed up trials considerably, by showing whether or not the drugs mentioned above have an actual effect and are working, before the fibrosis has a chance to decline and the testing becomes tougher to yield results of significance.
This photo shows the processes of myofibroblast activation:
1. HSCs reside in the space of Disse, which lies between the hepatocytes and endothelial cells of the sinusoid. Inactive HSCs store vitamin A and help to maintain normal liver function.
2. When the liver is injured, HSCs are activated by signaling molecules released by several cell types. These include damaged hepatocytes, the liver’s resident immune cells (a type of macrophage called Kupffer cells), infiltrating immune cells and other activated HSCs. HSCs then transform into myofibroblasts.
3. Myofibroblasts contract and exert tension on damaged tissue. They secrete collagen fibres and proteins such as elastin, which start to form scar tissue.
4. Collagen fibres accumulate and become cross-linked, stiffening the scar tissue.
Targeting intergrins on the surface on myofibroblasts
Targeting the formation of the fibre mesh
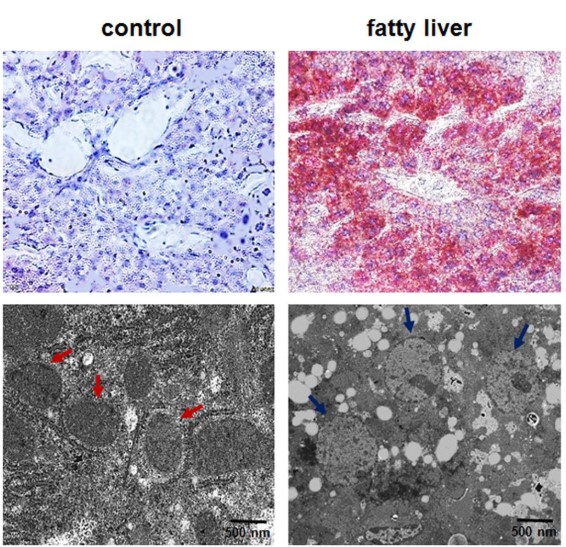
TEM Image of a fatty liver and a healthy control. Please note the fatty deposits on the below image within the fatty liver column, shown as multiple white dots, are not present on the corresponding image for the control.